Expert Mental Health Billing Services in New York – Get Paid Fast and Right
Managing a mental health practice in New York comes with unique financial and administrative challenges. Mental health billing services in New York are crucial for confirming your practice maintains consistent revenue while remaining compliant with state and federal regulations. From insurance verification to claim submission, payment posting, and denial management, every step requires precision and expertise. Our services are personalized to handle the complexities of behavioral health billing, allowing practitioners to focus entirely on patient care while we manage the financial operations with accuracy, routine wise processes, and detailed attention to detail.
Comprehensive Behavioural and Mental Health Medical Billing Services in New York
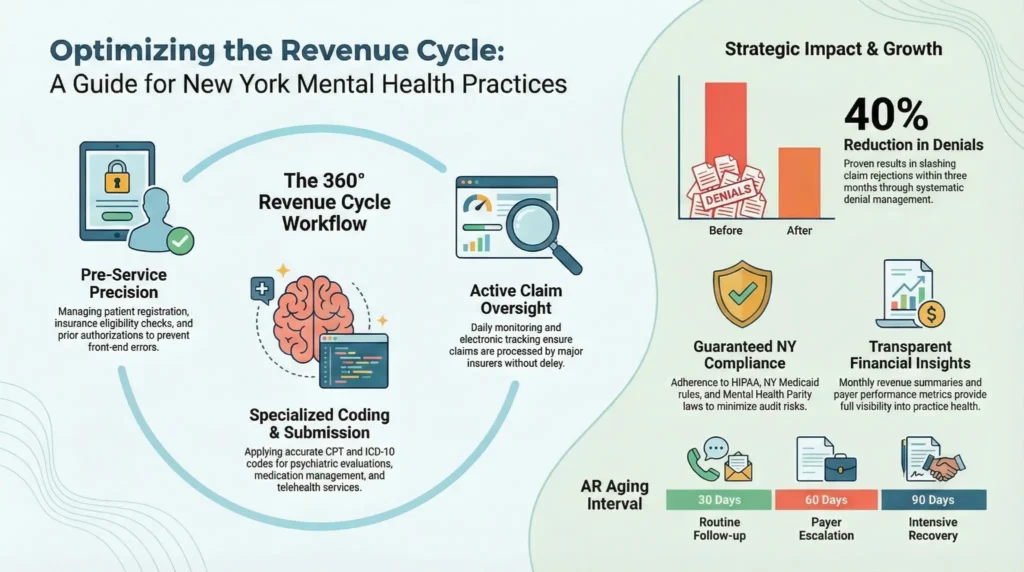
Behavioural and mental health services have unique billing requirements that differ from general medical practices. Our behavioural and mental health medical billing services in New York cover the full spectrum of administrative and financial needs. We manage everything from patient registration, insurance eligibility checks, and prior authorizations, to correct CPT and ICD-10 coding, electronic claim submission, payment reconciliation, and accounts receivable follow-up. Every claim is meticulously checked before submission to minimize errors and rejections. By handling billing routine wise and systematically, we help practices improve revenue consistency, reduce denials, and maintain smooth operations even as your patient volume increases. Behavioral health claims require additional attention to session types, duration, and documentation. We ensure that therapy sessions, psychiatric evaluations, medication management, and telehealth services are coded accurately and submitted in compliance with both payer-specific and state-specific requirements. Our team is well versed in New York Medicaid rules, commercial insurance plans, and Medicare guidelines for mental health services, which confirm your claims are processed without delay.
Mental Health Medical Billing Services in New York That Maximize Reimbursement
Cash flow stability is vital for mental health practices. Our mental health medical billing services in New York are designed to optimize reimbursements and reduce the time between service delivery and payment. We monitor claims daily, identify potential issues before submission, and follow up with insurance companies to ensure payments are processed efficiently. We work with major insurers such as Aetna, Cigna, UnitedHealthcare, and Blue Cross Blue Shield, as well as New York Medicaid managed care plans. By maintaining routine wise oversight of each claim, we prevent denials, recover lost revenue, and ensure your practice receives timely payments, keeping your operations financially secure. Our services include accurate patient statements, payment plan management, and electronic payment coordination. By managing patient billing clearly and efficiently, we enhance satisfaction and reduce confusion. Every payment is tracked, posted accurately, and reconciled to ensure that your practice maintains a transparent and reliable financial record.
Expert Mental Health Billing Services in New York – Get Paid Fast and Right
- Maximize Insurance Reimbursements – Accurate claim submission to reduce rejections and increase approvals.
- Faster Payments – Streamlined billing processes to improve cash flow and shorten payment cycles.
- Reduced Claim Denials – Proactive eligibility checks and error-free coding to minimize denials.
- Full Revenue Cycle Management – From patient verification to final payment posting.
- HIPAA-Compliant & Secure – Protecting sensitive patient data with strict compliance standards.
- Specialized in Mental Health Billing – Serving therapists, psychologists, psychiatrists, and counseling centers.
- New York Insurance Expertise – In-depth knowledge of NY payer rules and regulations.
- Dedicated Support Team – Personalized account management and real-time reporting.
Schedule Your Free Consultation
Revenue Cycle Management for Mental Health Providers
A complete revenue cycle management (RCM) approach is essential for modern behavioral health practices. Our team manages each stage of the revenue cycle, starting from patient registration and eligibility verification to final payment posting and financial reporting. By handling billing routine wise, we prevent errors and optimize collections. Our RCM services include:
- Patient registration and demographic updates
- Insurance verification and prior authorization
- Accurate CPT, HCPCS, and ICD-10 coding
- Electronic claim submission and tracking
- Payment posting and reconciliation
- Denial management and appeals
- Aging account reviews and collection follow-ups
This full-service approach confirm that your practice maintains financial health and compliance while freeing up valuable time for healthcare providers to focus on patient care.
Specialized Billing Solutions for Mental Health Practices
Mental health providers require highly specialized billing expertise. We customize our services to meet the needs of:
- Psychiatrists: Medication management, therapy sessions, and psychiatric evaluations require precise coding to maximize reimbursement and maintain compliance.
- Psychologists: Psychological testing, extended therapy sessions, and assessments require detailed documentation and coding accuracy to ensure clean claims.
- Licensed Clinical Social Workers (LCSWs) and Therapists: Individual, group, and family counseling services have unique billing and documentation requirements.
- Behavioral Health Clinics: Multi-provider practices benefit from high-volume claim management, payer-specific tracking, and routine wise reporting to maintain financial oversight.
By tailoring our services to your provider type and payer mix, we ensure smooth revenue cycle operations and reduce administrative stress for your staff.
Telehealth and Virtual Mental Health Billing Services in New York
With the rise of virtual healthcare, accurate telehealth billing has become crucial. Our team confirm that telehealth sessions are coded correctly with appropriate modifiers, place of service codes, and payer-specific documentation requirements. We routinely check session lengths, therapy types, and authorization requirements to ensure that telehealth claims are reimbursed efficiently. Proper management of virtual services guarantees that your practice can expand access to patients while maintaining predictable cash flow and compliance with New York State telehealth regulations.
Denial Management and Appeals to Protect Revenue
Denied claims can significantly impact practice income. Our routine wise denial management process includes thorough analysis, correction, and resubmission of claims. We investigate denial reasons, whether due to incorrect coding, missing documentation, or payer errors, and handle the appeal process from start to finish. By addressing denials proactively, we recover lost revenue, prevent recurring errors, and maintain smooth cash flow for your practice.
Compliance With New York Regulations
Compliance is critical in mental health billing. Our team confirm adherence to HIPAA, New York State Medicaid rules, mental health parity laws, and telehealth requirements. We routinely audit claims, documentation, and workflows to avoid penalties or audit risks. By keeping your billing process compliant, we protect your practice’s reputation and financial stability while allowing your staff to focus on patient care rather than regulatory issues.
Accounts Receivable Management for Consistent Cash Flow
Effective accounts receivable (AR) management is vital to maintaining strong financial health. Our team reviews unpaid claims, follows up with insurers routinely, and escalates pending accounts to recover funds professionally. We track aging reports at 30, 60, and 90-day intervals, confirming timely collection and reducing outstanding balances. By maintaining a proactive AR process, we help practices maximize revenue while minimizing administrative burden.
Transparent Reporting and Actionable Financial Insights
Our reporting system provides comprehensive, routine wise updates that give your practice full visibility into financial performance. Reports include monthly revenue summaries, claim status updates, denial trend analysis, payer performance metrics, and actionable recommendations for improvement. These insights allow you to make informed decisions, identify problem areas, and optimize revenue operations for long term growth.
Why Choose Our Mental Health Medical Billing Services in New York
We combine expertise, compliance knowledge, and routine wise billing processes to deliver unmatched service for mental health providers. Our advantages include:
- Dedicated billing specialists familiar with behavioural health practices
- Reduction in claim rejections and faster reimbursement cycles
- Routine wise monitoring of every claim and payment
- Secure, HIPAA-compliant billing systems
- Customized solutions for individual providers and multi-provider clinics
- Detailed reporting and financial insights to drive growth
Our team becomes an extension of your practice, confirming billing is handled efficiently, claims are paid accurately, and revenue cycles remain uninterrupted.
You Might Also Like
Expert Mental Health Billing Services in New York and Get Paid Fast and Right